LONSURF + bevacizumab extended survival and prolonged PFS
In the SUNLIGHT trial, patients treated with LONSURF + bevacizumab experienced approximately 11 months median overall survival and more than double the progression-free survival vs LONSURF alone.1,2
Study
population
(N=492)


(n=246)
LONSURF 35 mg/m2* orally,
twice daily Days 1-5 and 8-12
every 28 days
Bevacizumab 5 mg/kg by IV,
Days 1 and 15
(n=246)
LONSURF alone
35 mg/m2* orally, twice
daily Days 1-5 and 8-12
every 28 days


Treatment until disease progression, unacceptable toxic effects, or withdrawn consent
Follow-up every 8 weeks for radiologic progression and/or survival status
Primary endpoint
- OS
Secondary endpoints
- PFS
- ORR
- DCR
- Time to worsening
to ECOG PS ≥2 - Safety
Key inclusion criteria
- ECOG performance status (PS) of 0-1
- Disease progression or intolerance
- Histologically confirmed unresectable adenocarcinoma of the colon or rectum
-
No more than 2 previous chemotherapy regimens†
- Previous treatment must have included a fluoropyrimidine, irinotecan, oxaliplatin, an anti–vascular endothelial growth factor (VEGF) monoclonal antibody (not necessarily bevacizumab), or an anti–epidermal growth factor receptor (EGFR) monoclonal antibody (for patients with RAS wild-type disease)
- Known RAS status
Stratification
Randomization was stratified according to:
- Geographic region (North America, the European Union, or the rest of the world)
- Time since diagnosis of first metastasis (<18 months or ≥18 months)
- RAS status (wild type or mutated)
*Starting dose.2
†The treatment could have included neoadjuvant or adjuvant chemotherapy if disease had recurred during treatment or within 6 months after the last administration of neoadjuvant or adjuvant therapy.2
Key baseline characteristics2
| Characteristic | LONSURF + bevacizumab (n=246) | LONSURF (n=246) | |
|---|---|---|---|
| Age | Median, years (range) | 62 (20-84) | 64 (24-90) |
| <65 years, n (%) | 146 (59) | 129 (52) | |
| ≥65 years, n (%) | 100 (41) | 117 (48) | |
| Sex, n (%) | Male | 122 (50) | 134 (55) |
| Race or ethnic group, n (%) | White | 215 (87) | 220 (89) |
| Black | 4 (2) | 3 (1) | |
| Asian | 0 | 1 (<1) | |
| American Indian or Alaska Native | 1 (<1) | 0 | |
| Other | 8 (3) | 5 (2) | |
| Unknown | 18 (7) | 17 (7) | |
| Region, n (%) | European Union | 158 (64) | 157 (64) |
| North America | 8 (3) | 8 (3) | |
| Rest of the world | 80 (33) | 81 (33) | |
| Location of primary tumor, n (%) | Right side | 62 (25) | 77 (31) |
| Left side | 184 (75) | 169 (69) | |
| Time from diagnosis of first metastasis to randomization,a n (%) |
<18 months | 104 (42) | 105 (43) |
| ≥18 months | 142 (58) | 141 (57) | |
| RAS status,a n (%) | Mutant | 171 (70) | 170 (69) |
| Wild-type | 75 (31) | 76 (31) | |
| Prior treatment with anti-VEGF monoclonal antibody, n (%) | Yes | 178 (72) | 176 (72) |
| ECOG PS, n (%) | 0 | 119 (48) | 106 (43) |
| 1 | 127 (52) | 139 (57) | |
| 2 | 0 | 1 (<1)b | |
aData were determined from the interactive web-based response system used for randomization.2
bThe patient had an ECOG PS of 1 at randomization but was assessed as having a score of 2 on Day 1 of the first treatment cycle.2
Median duration of treatment2
months
months
At the time of the analysis,13% of the patients treated with LONSURF + bevacizumab and 1.6% treated with LONSURF alone were still receiving treatment.
PRIMARY ENDPOINT
~11 months mOS
Overall Survival (OS) (N=492)1,2
Hazard ratio (HR)=0.61, P<0.001
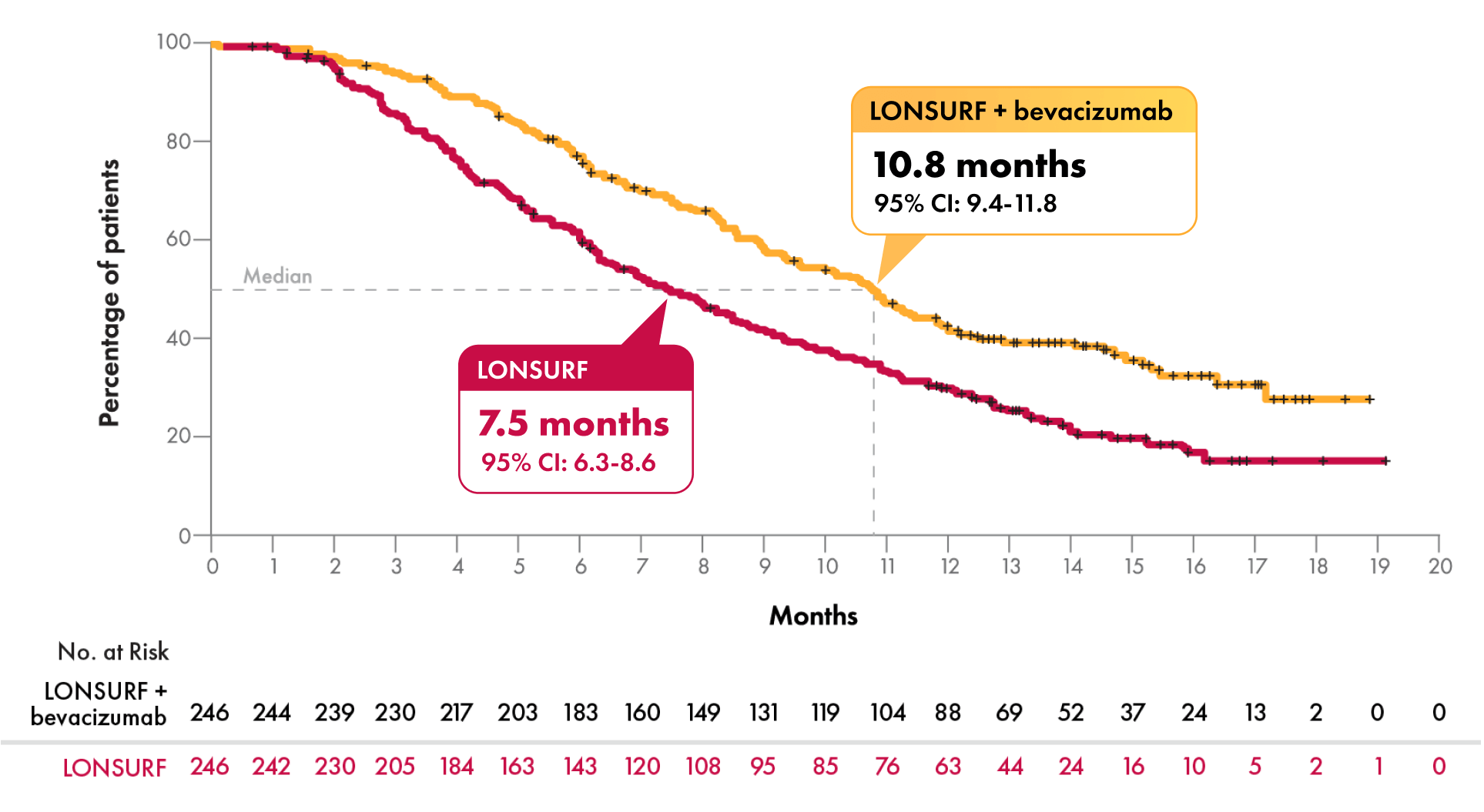


| OS comparison at key timepoints2,3 | 6 months | 12 months | 18 months |
|---|---|---|---|
| LONSURF + bevacizumab | 77% | 43% | 28% |
| LONSURF | 61% | 30% | 15% |
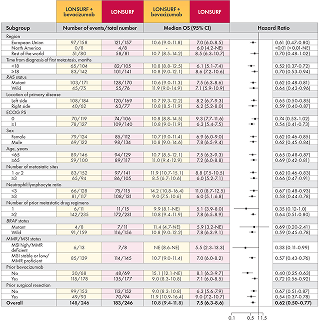
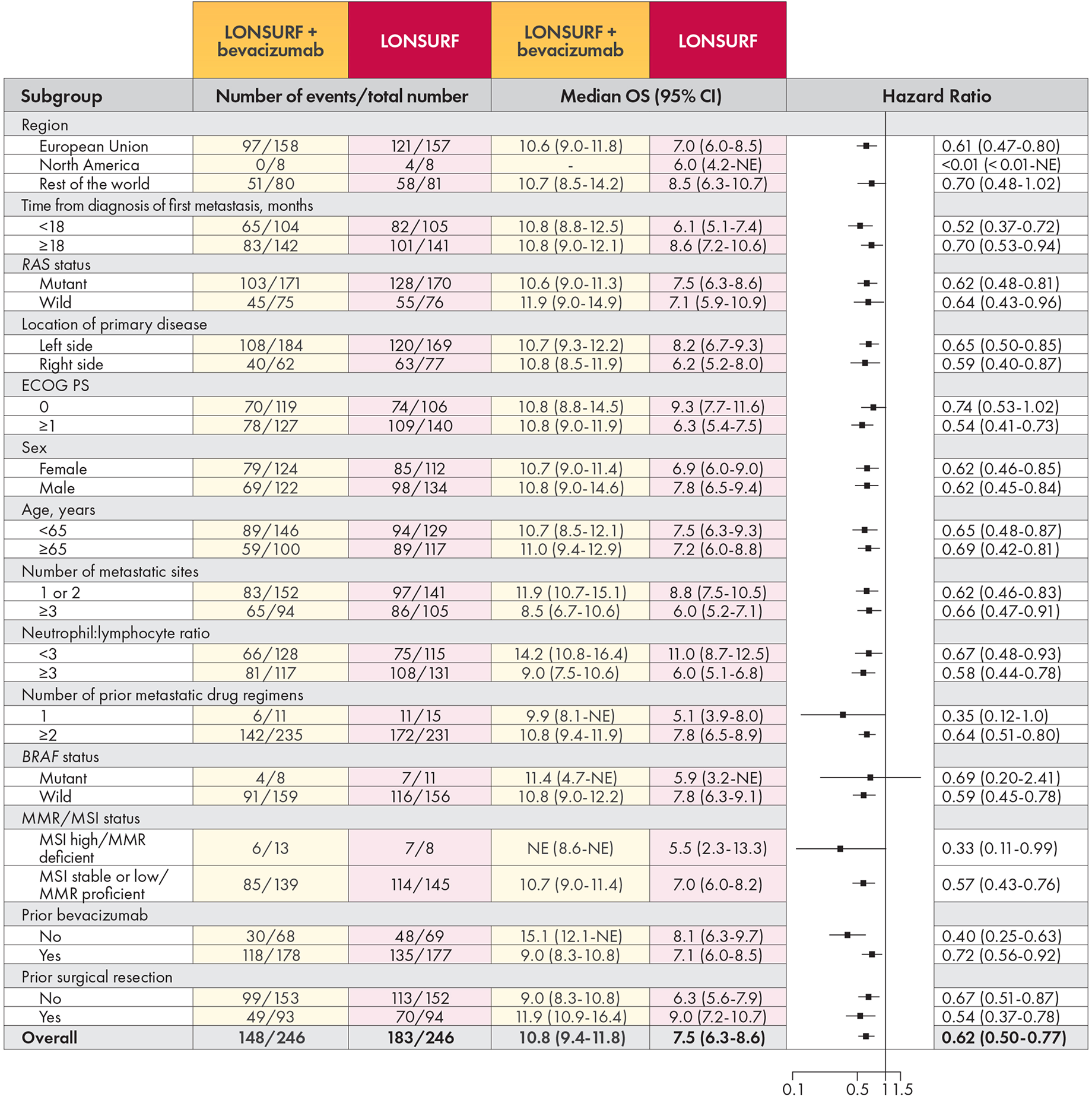
Within individual subgroups, it is difficult to apply statistical weight due to potential multiplicity issues, so these results should be interpreted with caution and no conclusions should be drawn.
MMR=mismatch repair; MSI=microsatellite instability; NE=not evaluable.
Results were consistent across all clinically relevant subgroups regardless of age, sex, location of primary disease, number of metastatic sites, RAS mutation status, and prior bevacizumab treatment.2
KEY SECONDARY ENDPOINT
Median PFS more than doubled
Progression-free Survival (PFS) (N=492)1,2
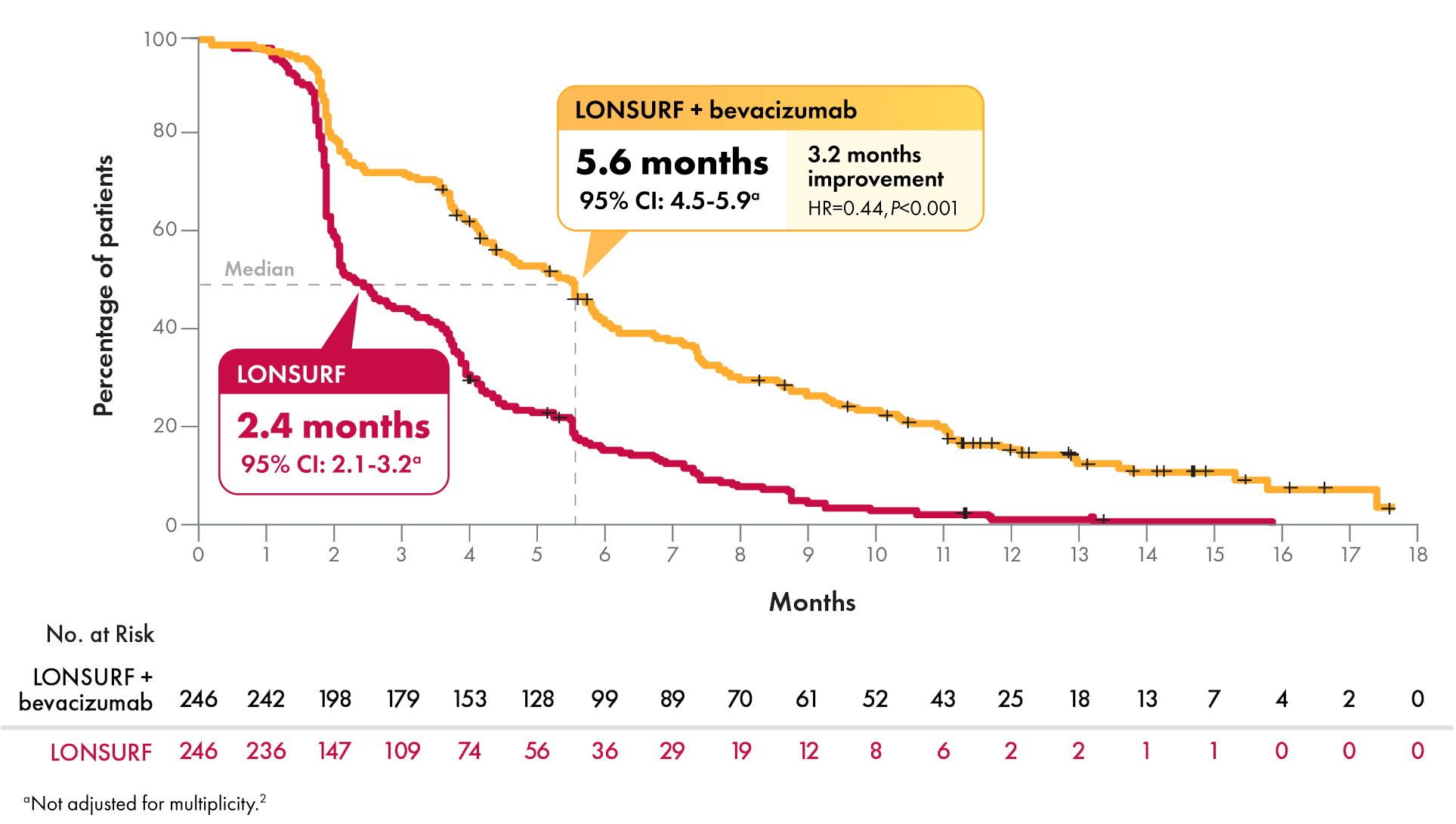


| PFS comparison at key timepoints2 | 6 months | 12 months | 18 months |
|---|---|---|---|
| LONSURF + bevacizumab | 43% | 16% | Not estimable |
| LONSURF | 16% | 1% | Not estimable |
At just under 16 months, PFS was 0% in the LONSURF arm vs 7.9% in the LONSURF + bevacizumab arm.

Within individual subgroups, it is difficult to apply statistical weight due to potential multiplicity issues, so these results should be interpreted with caution and no conclusions should be drawn.
MMR=mismatch repair; MSI=microsatellite instability; NE=not evaluable.
Results were consistent across all clinically relevant subgroups regardless of age, sex, location of primary disease, number of metastatic sites, RAS mutation status, and prior bevacizumab treatment.2
ADDITIONAL SECONDARY ENDPOINTS
More than three-quarters of patients achieved disease control4
Disease control rate (DCR)4
LONSURF +
bevacizumab
LONSURF
alone
Objective response rate (ORR)2
LONSURF +
bevacizumab
LONSURF
alone
DCR=objective response + stable disease; ORR=complete response + partial response.
Slower time to ECOG PS deterioration
Median Time to Worsening to ECOG PS ≥22,5*
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®)
NCCN
Recommended
The National Comprehensive Cancer Network® (NCCN®) recommends trifluridine and tipiracil (LONSURF) +/- bevacizumab as NCCN Category 2A recommended options for a potential third-line or subsequent treatment in mCRC patients. The trifluridine and tipiracil (LONSURF) + bevacizumab combination is preferred over trifluridine and tipiracil (LONSURF) alone.6,7
Category 2A=based upon lower-level evidence, there is uniform NCCN consensus (≥85% support of the Panel) that the intervention is appropriate.
NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Potential treatment algorithm for 3L use (KRAS/NRAS mutant)6
Initial therapy
FOLFOX +
bevacizumab
2L therapy
FOLFIRI +
bevacizumab
Subsequent therapies*
Trifluridine and tipiracil
(LONSURF) +/- bevacizumab
or
Fruquintinib, regorafenib,
clinical trials, or best supportive care
Potential treatment algorithm for 3L use (KRAS/NRAS wild type)6
Initial therapy
FOLFOX +
cetuximab
2L therapy
FOLFIRI +
bevacizumab
Subsequent therapies*
Trifluridine and tipiracil
(LONSURF) +/- bevacizumab
or
Fruquintinib, regorafenib,
clinical trials, or best supportive care
*Fruquintinib or regorafenib or trifluridine and tipiracil +/- bevacizumab are treatment options for patients who have progressed through all available regimens.
LONSURF is indicated as a single agent or in combination with bevacizumab for the treatment of adult patients with metastatic colorectal cancer previously treated with fluoropyrimidine‑, oxaliplatin‑ and irinotecan‑based chemotherapy, an anti‑VEGF biological therapy, and if RAS wild‑type, an anti‑EGFR therapy.
LONSURF is indicated for the treatment of adult patients with metastatic gastric or gastroesophageal junction adenocarcinoma previously treated with at least two prior lines of chemotherapy that included a fluoropyrimidine, a platinum, either a taxane or irinotecan, and if appropriate,


LONSURF is indicated as a single agent or in combination with bevacizumab for the treatment of adult patients with metastatic colorectal cancer previously treated with fluoropyrimidine‑, oxaliplatin‑ and irinotecan‑based chemotherapy, an anti‑VEGF biological therapy, and if RAS wild‑type, an anti‑EGFR therapy.
LONSURF is indicated for the treatment of adult patients with metastatic gastric or gastroesophageal junction adenocarcinoma previously treated with at least two prior lines of chemotherapy that included a fluoropyrimidine, a platinum, either a taxane or irinotecan, and if appropriate,
Severe Myelosuppression: In the 1114 patients who received LONSURF as a single agent, LONSURF caused severe or life‑threatening myelosuppression (Grade 3‑4) consisting of neutropenia (38%), anemia (17%), thrombocytopenia (4%) and febrile neutropenia (3%). Three patients (0.3%) died due to neutropenic infection/sepsis; four other patients (0.5%) died due to septic shock. A total of 14% of patients received granulocyte‑colony stimulating factors. In the 246 patients who received LONSURF in combination with bevacizumab, LONSURF caused severe or life-threatening myelosuppression (Grade 3‑4) consisting of neutropenia (52%), anemia (5%), thrombocytopenia (4%) and febrile neutropenia (0.4%). One patient (0.4%) died due to abdominal sepsis and two other patients (0.8%) died due to septic shock. A total of 29% of patients received granulocyte-colony stimulating factors. Obtain complete blood counts prior to and on Day 15 of each cycle of LONSURF and more frequently as clinically indicated. Withhold LONSURF for severe myelosuppression and resume at the next lower dosage.
Embryo‑Fetal Toxicity: LONSURF can cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to the fetus. Advise females of reproductive potential to use effective contraception during treatment and for at least 6 months after the final dose.
USE IN SPECIFIC POPULATIONSLactation: It is not known whether LONSURF or its metabolites are present in human milk. There are no data to assess the effects of LONSURF or its metabolites on the breastfed child or the effects on milk production. Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed during treatment with LONSURF and for 1 day following the final dose.
Male Contraception: Because of the potential for genotoxicity, advise males with female partners of reproductive potential to use condoms during treatment with LONSURF and for at least 3 months after the final dose.
Geriatric Use: Patients 65 years of age or older who received LONSURF as a single agent had a higher incidence of the following hematologic laboratory abnormalities compared to patients younger than 65 years: Grade 3 or 4 neutropenia (46% vs 32%), Grade 3 anemia (20% vs 14%), and Grade 3 or 4 thrombocytopenia (6% vs 3%). Patients 65 years of age or older who received LONSURF in combination with bevacizumab had a higher incidence of the following hematologic laboratory abnormalities compared to patients younger than 65 years: Grade 3 or 4 neutropenia (60% vs 46%) and Grade 3 or 4 thrombocytopenia (5% vs 4%).
Renal Impairment: No adjustment to the starting dosage of LONSURF is recommended in patients with mild or moderate renal impairment (CLcr of 30 to 89 mL/min). Reduce the starting dose of LONSURF for patients with severe renal impairment (CLcr of 15 to 29 mL/min) to a recommended dosage of 20 mg/m2.
Hepatic Impairment: Do not initiate LONSURF in patients with baseline moderate or severe (total bilirubin > 1.5 times ULN and any AST) hepatic impairment. Patients with severe hepatic impairment (total bilirubin > 3 times ULN and any AST) were not studied. No adjustment to the starting dosage of LONSURF is recommended for patients with mild hepatic impairment.
ADVERSE REACTIONSSerious adverse reactions occurred in 25% of patients. The most frequent serious adverse reactions (≥2%) were intestinal obstruction (2.8%), and COVID-19 (2%). Fatal adverse reactions occurred in 1.2% of patients who received LONSURF in combination with bevacizumab, including rectal fistula (0.4%), bowel perforation (0.4%) and atrial fibrillation (0.4%).
The most common adverse reactions or laboratory abnormalities (≥10% in incidence) in patients treated with single‑agent LONSURF at a rate that exceeds the rate in patients receiving placebo in mCRC: anemia (77% vs 33%), neutropenia (67% vs 0.8%), asthenia/fatigue (52% vs 35%), nausea (48% vs 24%), thrombocytopenia (42% vs 8%), decreased appetite (39% vs 29%), diarrhea (32% vs 12%), vomiting (28% vs 14%), abdominal pain (21% vs 19%), and pyrexia (19% vs 14%). In metastatic gastric cancer or gastroesophageal junction (GEJ): neutropenia (66% vs 4%), anemia (63% vs 38%), nausea (37% vs 32%), thrombocytopenia (34% vs 9%), decreased appetite (34% vs 31%), vomiting (25% vs 20%), infections (23% vs 16%) and diarrhea (23% vs 14%).
Pulmonary emboli occurred more frequently in LONSURF‑treated patients compared to placebo: in mCRC (2% vs 0%) and in metastatic gastric cancer and GEJ (3% vs 2%).
Interstitial lung disease (0.2%), including fatalities, has been reported in clinical studies and clinical practice settings in Asia.
The most common adverse reactions or laboratory abnormalities (≥20% in incidence) in patients treated with LONSURF in combination with bevacizumab vs LONSURF alone were neutropenia (80% vs 68%), anemia (68% vs 73%), thrombocytopenia (54% vs 29%), fatigue (45% vs 37%), nausea (37% vs 27%), increased aspartate aminotransferase (34% vs 28%), increased alanine aminotransferase (33% vs 23%), increased alkaline phosphate (31% vs 36%), decreased sodium (25% vs 20%), diarrhea (21% vs 19%), abdominal pain (20% vs 18%), and decreased appetite (20% vs 15%).
References: 1. LONSURF [package insert]. Princeton, NJ: Taiho Oncology, Inc.; 2023. 2. Prager GW, Taieb J, Fakih M, et al. Trifluridine‑tipiracil and bevacizumab in refractory metastatic colorectal cancer. N Engl J Med. 2023;388(18):1657-1667. 3. Data on file. Taiho Oncology Inc., Princeton, NJ. 4. Fakih M, Prager GW, Tabernero J, Amellal N, Calleja E, Taieb J. Clinically meaningful outcomes in refractory metastatic colorectal cancer: a decade of defining and raising the bar. ESMO Open. 2024;9(11):103931. 5. Taieb J, Fakih M, Tabernero J, et al. Impact of treatment with trifluridine/tipiracil in combination with bevacizumab on health-related quality of life and performance status in refractory metastatic colorectal cancer: an analysis of the phase III SUNLIGHT trial. Published online December 11, 2024. 6. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Rectal Cancer V.2.2025. © National Comprehensive Cancer Network, Inc. 2025. All rights reserved. Accessed June 5, 2025. To view the most recent and complete version of the guideline, go online to NCCN.org. 7. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Colon Cancer V.3.2025. © National Comprehensive Cancer Network, Inc. 2025. All rights reserved. Accessed June 5, 2025. To view the most recent and complete version of the guideline, go online to NCCN.org.
